COVID-19 in practice
SARS-CoV-2 to its friends
2020-11-24 — 2022-12-07
Wherein the limits of rapid antigen tests for Omicron are examined, with saliva PCR cycle-threshold discordance noted, throat swabbing and CO2 ventilation monitoring are considered, and microlife-style risk calculators are recommended.
This notebook is retired. See Respiratory viruses in practice for an updated treatment.
1 Epidemiology of
See also epidemiology, contact tracing.
2 Testing dynamics
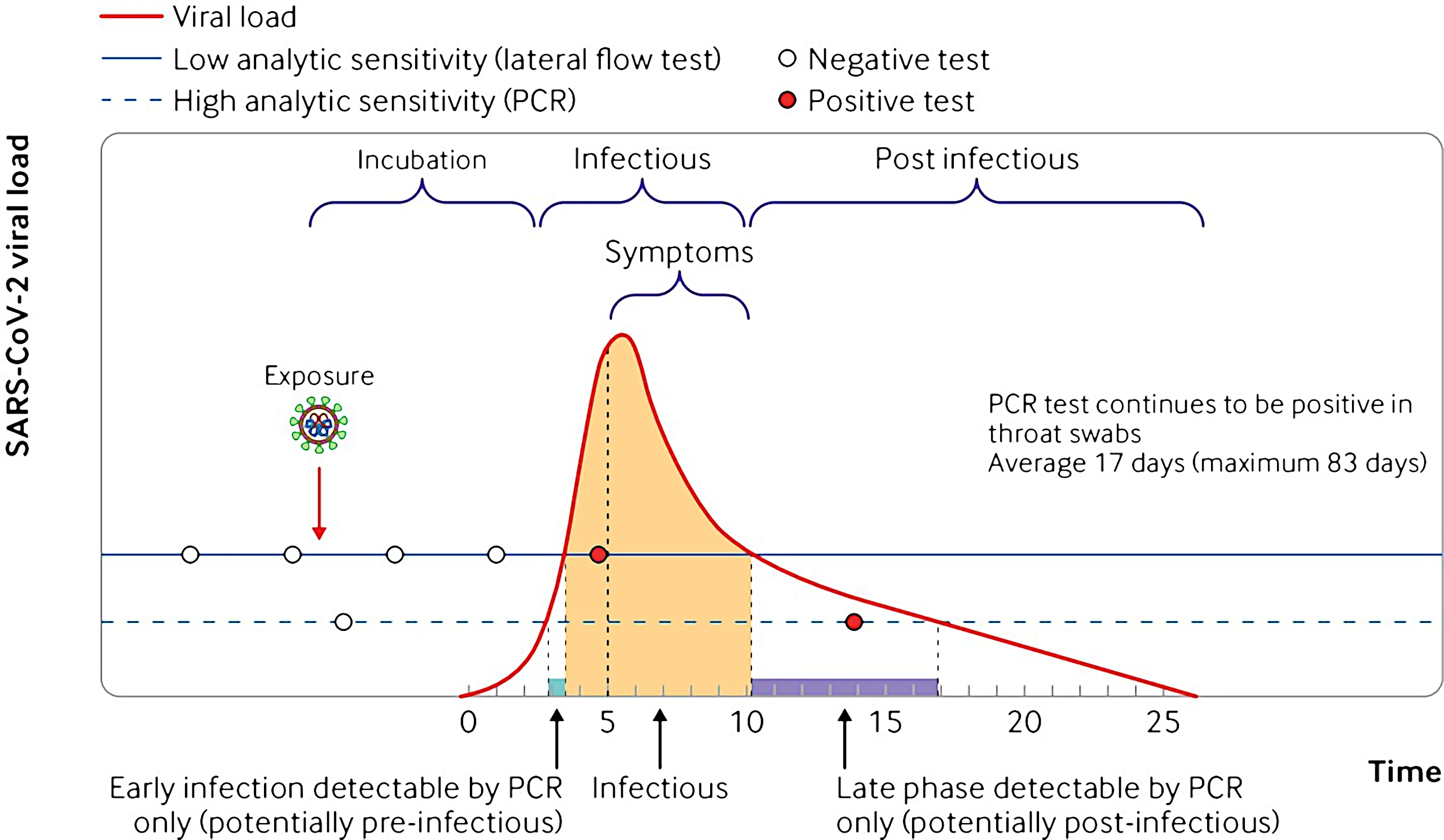
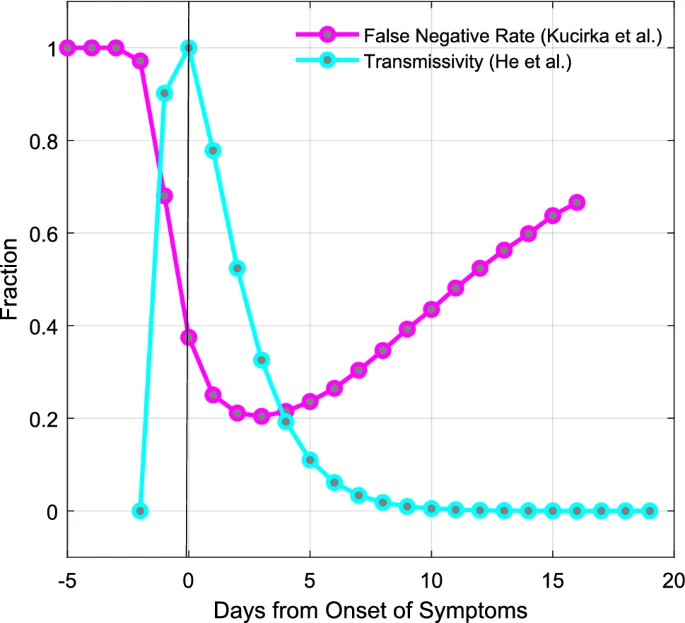
Current public health advice boils down to a heuristic that the Rapid Antigen Tests (🐀) are a good proxy for actual contagiousness.
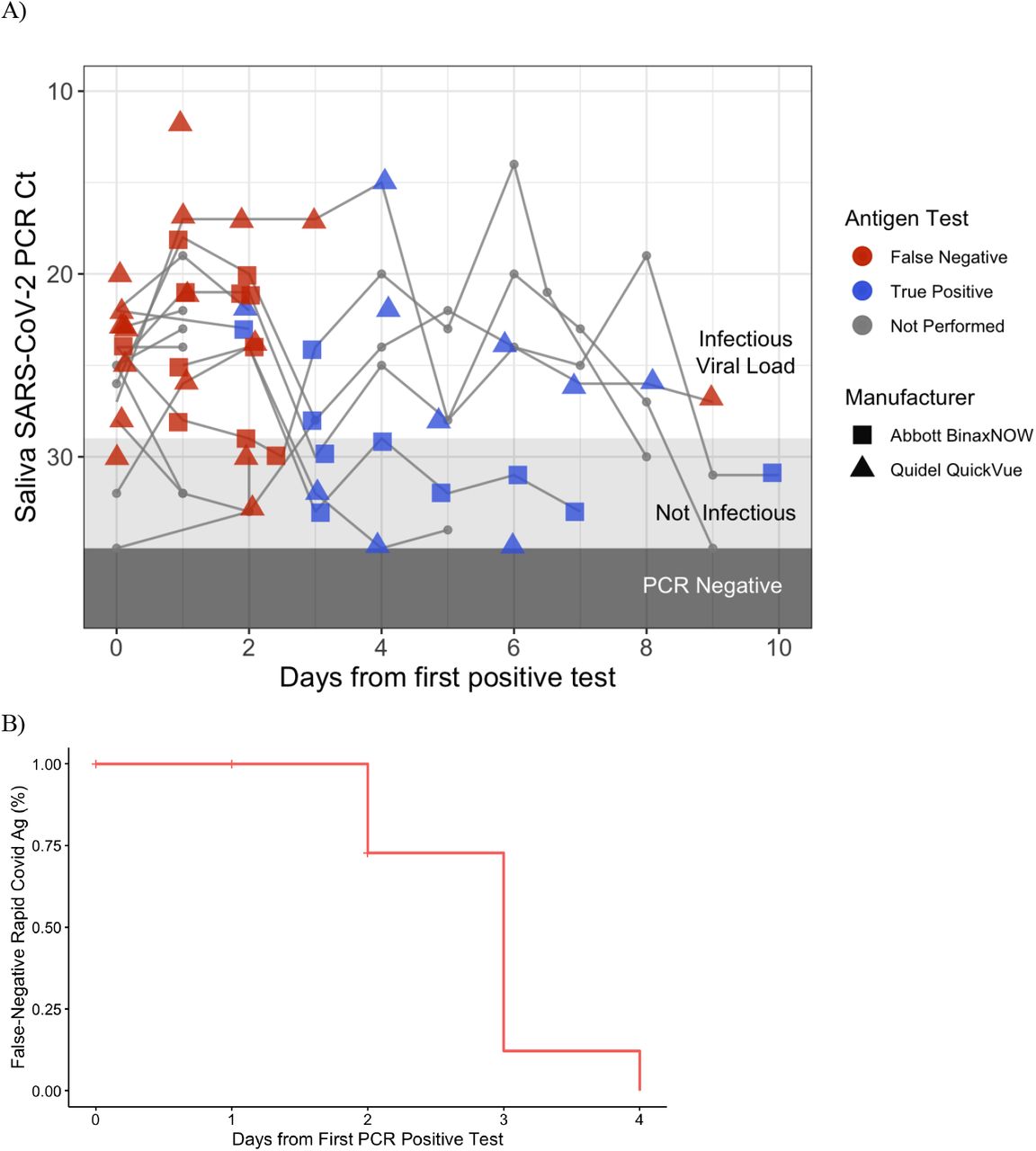
The actual story is complicated and nuanced. Small sample trial, updated for Omicron: Adamson et al. (2022), observes Covid transmission with saliva PCR cycle threshold (Ct) values between 23-28 for the N gene in an \(n=30\) trial. tl;dr: For their tests at least the start of the infection window was not detected by 🐀s (all false negatives.) At the end of the infection, 🐀s produce both false positives and false negatives wrt/ infectiousness. Data here.
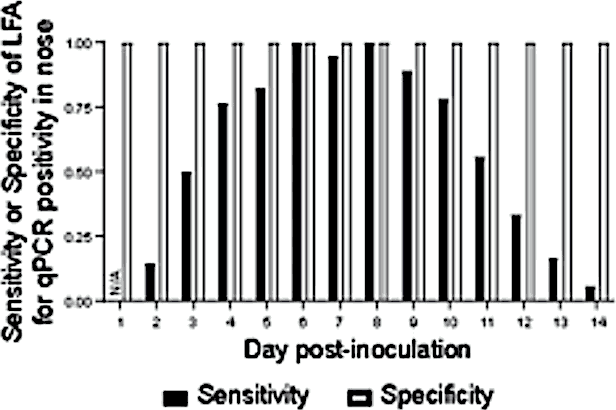
Bonus complication: we are possibly using 🐀s wrong, at least for Omicron, if we follow the advice to swab only our noses. Should you add a throat swab to your at-home covid test?. update: This is ambivalently helpful and may even get a false positive (Killingley et al. 2022). Here is a new graph of test efficacy from that study, which was small but well controlled (it was the first challenge trial).
3 Personal risk calculators
For now, as a good tool for thinking things through (very approximately!) I recommend a microlife-style COVID risk calculator to consider the risk of various activities.
- microCOVID Project
- microcovid Data if you feel like updating it
I find it clarifying, although I do not take it literally. Obviously, check the dates and specificity of the data for your region, and bear in mind that it is just an estimator, and written by non-epidemiologists. For example, there is something funky about how they account for the duration of activities; my risk for catching covid should asymptotically approach a constant as time goes on, but it seems to increase linearly? That approximation is probably fine for many events of interest, but use care in planning long events.
3.1 Airborne transmission
Elizabeth van Nostrand recommends the Bazant lab COVID-19 Indoor Safety Guideline (Bazant and Bush 2021) for a risk calculator for indoor events. Here is the source code for that and here is the model.
See also p CO2 monitoring.
- Portable CO2 meters could be used to help fight coronavirus transmission, experts say
- CO2 monitoring recommended to manage COVID-19 spread in schools and offices
(Burridge et al. 2021; Bazant et al. n.d.; Bazant and Bush 2021)
The backstory to how this has been mishandled is fascinating (Randall et al. 2021; C. C. Wang et al. 2021): The 60-Year-Old Scientific Screwup That Helped Covid Kill.
4 Evaluating societal cost
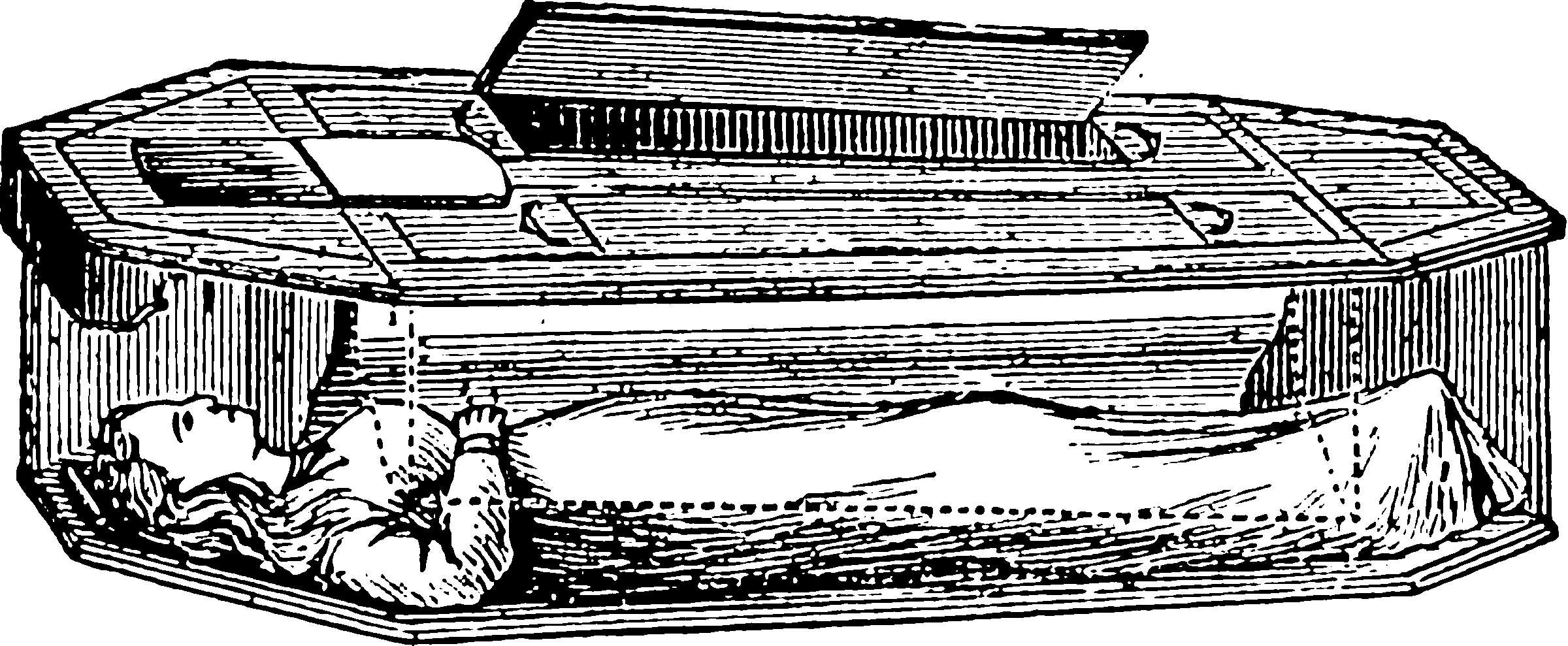
Actuarial lives and quality-adjusted-life-years were not popular for costing public interventions in the pandemic (Hall and Viney 2021). Subhash Pokhrel explains at length Why standard ways of valuing health were set aside during the pandemic. He argues, basically, that we use a risk-averse decision rule to value public interventions as a kind of precautionary principle. Implicitly, this leads us to ask, why did we not do better experiments to reduce uncertainties so we could make that trade-off better? It seemed that uncertainty was extremely expensive and therefore that we had a massive budget to reduce it. This is the platform of organisations like 1Day Sooner who advocate accelerated medical trials by participants who volunteered to be infected. I volunteered for this.
Human challenge trials deliberately expose participants to infection, to study diseases and test vaccines or treatments.
This is cheap talk though. There was not really anywhere to take my volunteer energy in Australia, and thereby prove that I would put my money where my mouth is on this.
Now that we have acquired more precise estimates of COVID dynamics, Paul Dolan and Christian Krekel advocate a return to QALY-like measures in How should we measure the impact of Covid-19 policies on our wellbeing?; There are some nifty links in the citation list.
I am curious about the risk of new variants of COVID and the implications of the new regime. I do not know enough epidemiology or virology to understand the risks we face there, but I suspect it is going to be a classic Black swan tail-risk (Cirillo and Taleb 2020). That is, we want to account for the possibility of large extreme downsides to whatever policies we adopted.
Optimising for Expected QALY is not enough if it comes with a significant risk of extreme QALY loss. That said, the economic consensus is strongly against substantial public health interventions at this stage.
Also, the question of how to trade-off wellbeing, happiness and disease risk is tricky and deep. To read: Dolan and Kahneman (2008) on what hedonism even is.
5 Virulence and risks upon infection
5.1 Death and life years
As measured by lost lifetime, some COVID deaths are crueller than others. When a 90-year-old victim with multiple health complaints goes one month earlier to their grave because of COVID, that is sad, but it is not so awful as when a child is cut down decades early. Mercifully, COVID vastly prefers the former case to the latter — it is more likely to scrape some time off the end of a long life than to cut down a short one. So, if some of us die of COVID, how much of my life will it have cost me, on average? Wouterse, Ram, and van Baal (2022) we would have lost 3-4 quality-adjusted life years (QALY) on average. This was before Omicron and may need updating, if the age profile has changed substantially.
5.2 Relative rate compared to normal life risk
We might wonder how much catching COVID adds to your risk rate. Back before Omicron David Spiegelhalter asked How much ‘normal’ risk does Covid represent? and answered (Spiegelhalter 2020)
roughly speaking, we might say that getting COVID-19 is like packing a year’s worth of risk into a week or two.
In fact it is complicated, with slightly more risk for over 55s and much less for 20 school children.
5.3 Long covid
Seems to be real, dammit (Blomberg et al. 2021). Well then, how bad is it? How much risk of it should I tolerate? Elizabeth Van Nostrand argues Long Covid Is Not Necessarily Your Biggest Problem, i.e. that it is a real problem but does not loom particularly large amongst in all the other real problems. Scott Alexander that it looms reasonably large. There has been a methodological update which revises the probability of long covid symptoms down: UK Office for National Statistics: Technical article: Updated estimates of the prevalence of post-acute symptoms among people with coronavirus (COVID-19) in the UK. It is not compactly summarised in that report, but you can scroll down a Zvi Mowshowitz article to find highlights.
As far as long-ish COVID, i.e. all the other non-death inconveniences, a report based on Maltese data (Cuschieri et al. 2021) estimates that 95% of the impact of COVID in Disability-adjusted life years from 2020 is being dead; the remaining 5% is other stuff. The report is also pretty interesting as far as working out how much of the impact of sickness is tiredness after the initial phase etc. They argue that the community impacts of long term COVID are probably somewhat higher than the acute impacts of COVID, although not by much. Worth a read.
🚧TODO🚧 clarify: C&C with Long influenza
5.4 Comorbidities
5.5 Omicron variant
Why are we slow to pump out relative morbidity estimates for the notionally civilization-defining moment of Omicron dominance?
Best I could find was Lewnard et al. (2022) which doesn’t break out the relative morbidity versus vaccine, except to note omicron sufferers were more likely to be vaccinated than delta sufferers. Across all patients
Omicron variant infections were associated with 52%, 53%, 74%, and 91% reductions in risk of any subsequent hospitalization, symptomatic hospitalization, ICU admission, and mortality, relative to Delta variant infections. Median duration of hospital stay for patients admitted with symptomatic Omicron variant infections was approximately 70% (∼3.4 days) shorter than that observed among patients with symptomatic Delta variant infections.
Realistically, this means we can estimate the mortality risk from Omicron as around 4-5 days of normal risk.
6 Transmission
I need to collect some articles on these themes, when I have a moment to spare.
Which interventions are best? Jeremy Howard summarises lower cost interventions: improved masks, better ventilation, rapid antigen testing.
A cursory inspection of the literature seems to suggest that surface transmission is not worth worrying about (but why not wash your hands?)
Transmission comes down mostly to airflow, afaict. Where are those airborne virions going?
Masking well is hard, but seems to make a difference if you do it well. Evidence for masking lazily (i.e. like a normal human) seems pretty weak.
Distancing is not entirely pointless but effectiveness depends on airflow.
What is easy to do well and makes a difference is ventilation. Do things outside if possible. Do things with the windows open if possible. If the windows don’t open, check that the aircon has a HEPA filter. If the aircon does not have a filter, just get an air purifier. They are not that expensive. I have a Breville the Easy Air Purifier, although I have not assayed its effectiveness against COVID-19 specifically. At AUD229, its ticket price is less than the cost of skipping work for a week due to COVID.
Questions: Does UV air purification do the trick, e.g. here is a UVC Air Purifier for HVAC. Since I have presented these assertions without evidence, please don’t take them on trust. Supporting citations or refutations welcome.
6.1 Modelling airborne transmission
Is the Wells-Riley model any good? (Noakes and Sleigh 2009; Sze To and Chao 2010).
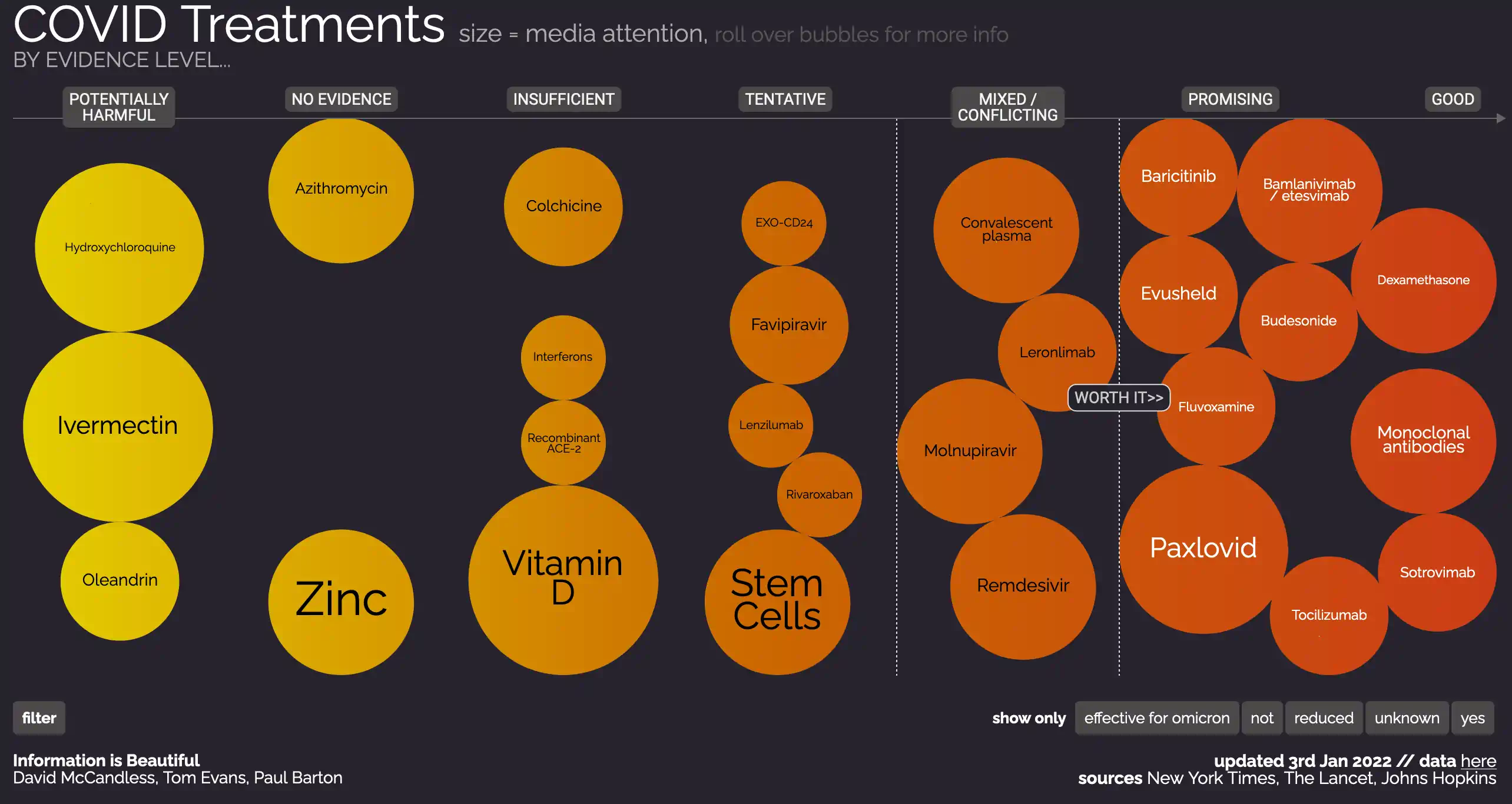
7 Treating
A contentious area.
There is a reasonably current overview of various options in 11-16-2021_JHMI Clinical Recommendations for Pharmacologic Treatment of COVID-19. Notably includes several off-the-shelf treatments. I’m not even listing the monoclonal antibodies.
- Fluvoxamine, a.k.a. Prozac (!) (Berwanger 2022; Reis et al. 2022)
- NIH COVID-19 Treatment Guidelines
- High-dose budesonide for early COVID-19
- Dexamethasone, an inexpensive and widely available steroid, NHS England » COVID treatment developed in the NHS saves a million lives
- Tocilizumab and sarilumab alone or in combination with corticosteroids for COVID-19: A systematic review and network meta-analysis
7.1 Topical sprays
Various nasal sprays are used for cold and other viruses, some of which might have an effect on COVID (Fais et al. 2022; Friedland et al. 2022; Fröba et al. 2021; Kozlov 2022).
One ingredient which has specific clinical trials for covid Nitric Oxide (Salman 2021) which has passed clinical trials (Sanotize Research and Development corp. 2021; Winchester et al. 2021) and been released as a product, Enovid/VirX in a slow-release nasal spray formulation.
enovid and VirX are the identical product, branded under different names for marketing in various territories around the world. Nitric Oxide Nasal Spray (NONS) is the generic name of the product.
7.2 Vitamin D
Wow, why is the Vitamin D literature so spammy?
- Dr. Fauci takes 6,000 IU of Vitamin D daily
- Vitamin D Nearly Abolishes ICU Risk in COVID-19
- Vitamin D Flops in Moderate-Severe COVID
tl;dr; AFAICT the case that Vitamin D is helpful is weak, and the case that it is not hurtful is strong so, take vitamin D if you want.
8 Simulating
- ViraTrace/InfectionModel: Code for the ViraTrace infection model.
- BDI-pathogens/OpenABM-Covid19: OpenABM-Covid19: an agent-based model for modelling the spread of SARS-CoV-2 (coronavirus) and control interventions for the Covid-19 epidemic
- zalandoresearch/CRISP: A probabilistic graphical model for COVID-19 infection spread through a population based on mutual contacts between pairs of individuals across time as well as test outcomes. The C++/Python implementation enables full inference at the scale of millions of contacts between thousands of individuals.
- Making Sense of COVID-19 through Simulations
- What Happens Next? COVID-19 Futures, Explained With Playable Simulations
- chrisbillington.net’s simple smoothing model (python source code)
- zappingseb/coronashiny: A shiny app visualising corona data
- Covid-19: the SPQEIR model
- Assessing suppression strategies against epidemic outbreaks like COVID-19: the SPQEIR model
- R Epidemics Consortium Projects
- CBDRH/covoid: COVID-19 Open-source Infection Dynamics
9 Current restrictions where I live
Too confusing, gave up trying to understand. I gave up and prioritise following empirical estimates of safety from illness rather than safety from legal trouble.